Communities to the rescue
 community participation can work wonders , especially when it comes to tackling diseases like malaria. The Zimbabwe experience in recent years shows that, in what otherwise appears to be a hopeless situation, communities can reverse the fortunes of thousands of people susceptible to the disease.
community participation can work wonders , especially when it comes to tackling diseases like malaria. The Zimbabwe experience in recent years shows that, in what otherwise appears to be a hopeless situation, communities can reverse the fortunes of thousands of people susceptible to the disease.
Also referred to as a disease of the poor, millions die each year as a result of malaria and, in most cases, the deaths result from ignorance of how to deal with it. Only a few countries have the resources to deal with the disease effectively at the governmental level. It is due to this that people often ignore the fact that existing resources could help.
Many countries have developed a dependency syndrome and often adopt only token efforts to deal with the disease. Many wait for donor resources to be available to tackle the menace.
Community management of such diseases are never considered because there is a misconception that malaria can only be controlled by experts and that local people are not educated or clever enough to sort out problems for themselves.
A malaria community-based management project was introduced in parts of Zimbabwe in 1994. The Department for International Development and Save the Children Fund worked in conjunction with the country's ministry of health.
It started as a small project in which malaria control was made part of the school curriculum. Schoolchildren were taught to recognise mosquito breeding sites within one kilometre of the school. Environmental control techniques, such as filling up pools of dispensable water and deepening edges of large ponds or streams where mosquitoes might breed, were adopted. Where this was not possible, larvicides were used. In some schools, this was so successful that it was possible to sleep outside at night without a single mosquito hovering around even during the peak rainy season, when the incidence of malaria is highest.
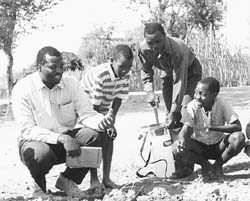
The concept of the school programme was then expanded to include the local people. Local health officials were taught every method to destroy mosquito breeding sites and how to mobilise community members. The only inputs that had to be procured were spray pumps and larvicides. In time, community volunteers from remote areas were taught how to treat malaria and were supplied with chloroquine. Only small children or complicated cases were referred to a doctor.
The programme has now been running for five years in two districts in the Zambezi Valley, where malaria is rampant. The methods employed have proved popular with both the public and the local health authorities, who now manage the programme. Community participation is part of the overall policy to deal with malaria in both districts.
The success of the programme is evident in both districts as malaria is now managed completely at the district level. In the Zambezi Valley, two examples demonstrate what can be achieved through community mobilisation. In one situation, both districts managed to deal with malaria outbreaks internally, while surrounding districts needed extensive external support. At one clinic, malaria control was carried out solely by using larvicides. Six weeks later, the local clinic staff had little to do and were found spending their time reading newspapers. At the same time, surrounding clinics in the same districts had queues of over 100 patients each awaiting treatment.
In another example, malaria prevalence rates were reduced by 50 per cent in one year. However, the following year, it went down by only 5 per cent. The only problem with community-based management is that communities are not paid, so they cannot be fired if they fail. Participation levels also vary from one area to another, depending on a number of factors. This is not to say that community participation will fail in some cases. It just means that some communities take more time. However, once a community is mobilised, thousands of people come forward to deal with the problem.
The Zimbabwean malaria projects have demonstrated that given the right set of circumstances and motivation, community participation can give real and lasting results.
This concept has now been taken to Afghanistan. The project, funded by the European Union and implemented by Healthnet International, was only started recently, but Afghan villagers have proved just as willing (or even more so) to adopt the methodology once they recognise the problem for themselves.
The author is malaria programme coordinator, Healthnet International, Jalalabad, Afghanistan
Related Content
- The Sustainable Development Goals Report 2023: special edition
- The double burden of COVID-19 and locusts in East Africa: Saving Millions of People From Hunger and Malnutrition
- Nepal State of Environment Report: The Monthly Overview, November, 2014
- Floods on different rivers in Kanchanpur displace more than 600 families
- China quake toll climbs to 207 as rescue teams search for survivors
- Fuel shortage adds to storm woes in US
